What does “going out of network” mean for me?
When your health care provider “goes out of network”, it means they don't have a contract with your insurance plan to provide services. You are still insured, but out-of-pocket costs may increase if you use out-of-network providers.
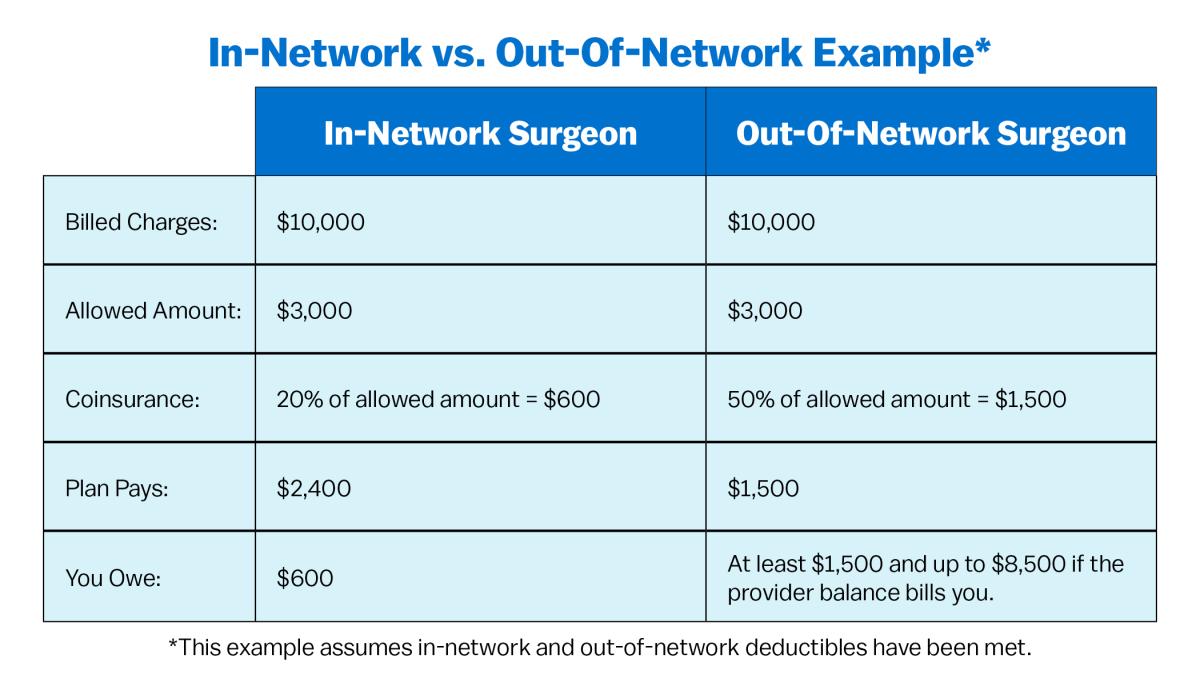
Understanding networks and out-of-pocket costs is important. To help you better understand networks and out-of-network costs, here are some key points to keep in mind:
- In-network providers typically have lower out-of-pocket costs than out-of-network providers.
- If you see an out-of-network provider, you may be responsible for paying the difference between the provider's charges and what your insurance company will pay.
- Some plans offer out-of-network coverage, which may come with higher deductibles, copays, and coinsurance amounts.
- If you have a specific provider or facility in mind, it's important to check if they are in-network before scheduling an appointment.
- When traveling, it's important to understand your plan's out-of-network coverage.
Image
Some exceptions:
- Emergency Services: A facility or a provider may not bill you more than your in-network cost sharing amounts for emergency services, even if the facility providing the emergency services is out-of-network. If you are experiencing an emergency, don't hesitate to seek immediate medical attention even if the provider is not in your network.
- Specialty Care: Sometimes, you need to see an out-of-network provider because specialized care is unavailable in your network. This may require your insurance company to provide prior authorization before your services are approved for payment, or to make other arrangements for you to get the care you need. Talk to your doctor and insurance company to determine your options.
Definitions
Helpful Links
